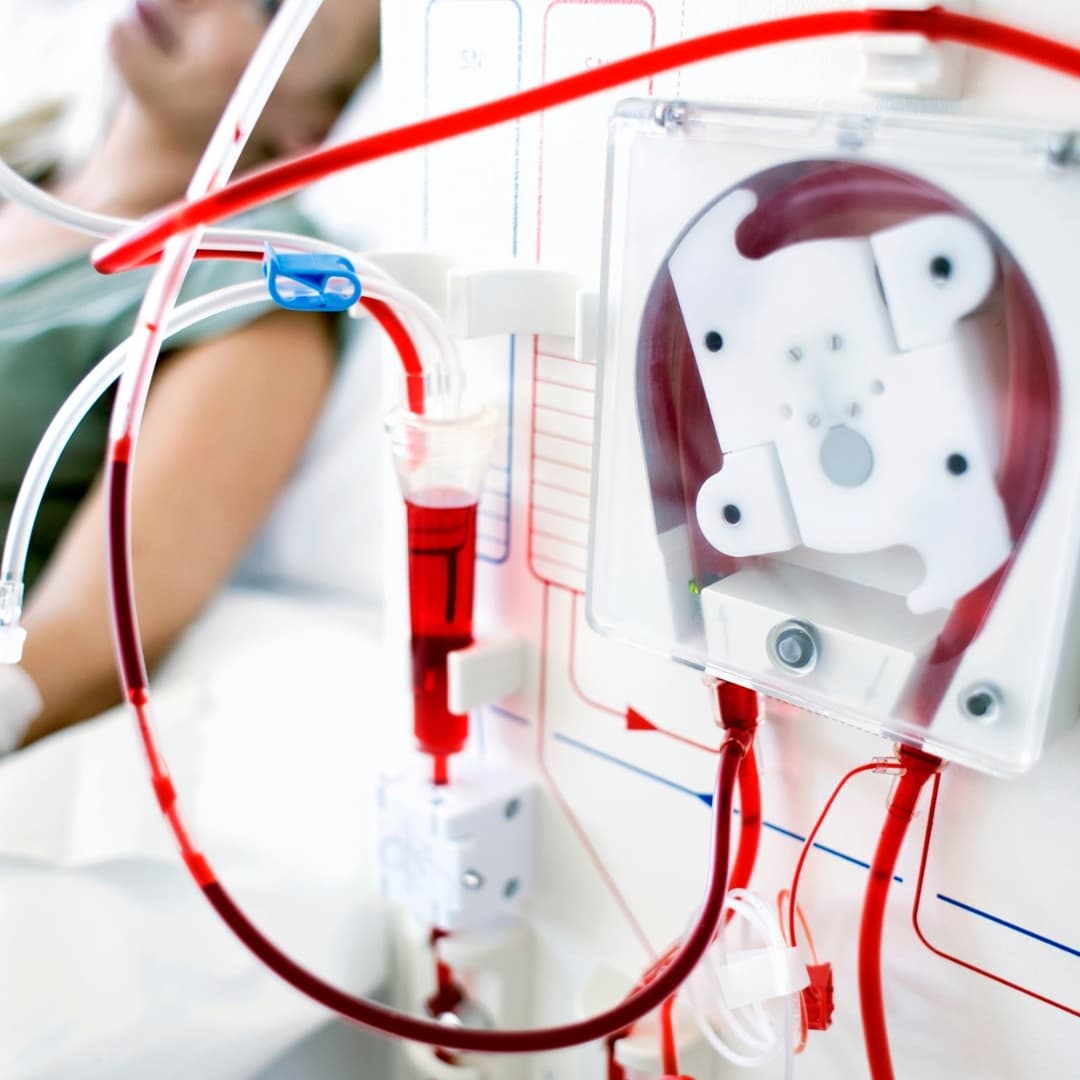
Dialysis Care (Hemodialysis & Peritoneal Dialysis)
Dialysis is a life-saving treatment for patients whose kidneys can no longer filter waste and excess fluid from the blood. It can be done through Hemodialysis, where blood is cleaned using a dialysis machine, or Peritoneal Dialysis, where a cleansing fluid is used inside the abdomen. Dialysis helps patients manage symptoms and maintain quality of life until a kidney transplant is possible.
When Dialysis May Be Needed
- Persistent nausea, vomiting, or loss of appetite.
- Severe swelling in legs, feet, or around the eyes.
- Extreme tiredness and weakness.
- Shortness of breath or chest pain due to fluid buildup.
- Confusion, difficulty concentrating, or poor sleep.
- Declining kidney function test results (eGFR, creatinine).
Why Dialysis Is Needed
- Chronic Kidney Disease (CKD) progressing to end-stage renal failure.
- Acute Kidney Injury (AKI) not improving with other treatment.
- Uncontrolled high blood pressure causing kidney damage.
- Diabetes-related kidney disease.
- Polycystic Kidney Disease (PKD) or other hereditary conditions.
- Severe urinary obstruction or repeated kidney infections.
Do's & Don'ts for Hemodialysis & Peritoneal Dialysis
- Do's
- Attend all scheduled dialysis sessions without fail.
- Follow a kidney-friendly diet with limited salt, potassium, and phosphorus.
- Take prescribed medicines on time.
- Keep dialysis access (fistula or catheter) clean and safe.
- Stay active and maintain regular follow-up with your nephrologist. Don'ts
- Don't skip or shorten dialysis sessions.
- Avoid excess fluid intake beyond your doctor's advice
- Don't eat high-salt, high-protein, or processed foods.
- Avoid lifting heavy objects with your fistula arm.
- Don't ignore signs of infection such as fever, redness, or swelling.
